96372 cpt code description
Please visit TheraNest on www. Read about Why we rebranded. Understanding how and when to use the CPT code can help you optimize 96372 cpt code description billing process. When it comes to mental and behavioral health billing, using codes to correctly bill for the services you deliver to your patients is a crucial component to getting paid on time.
CPT Code information is available to subscribers and includes the CPT code number, short description, long description, guidelines and more. Save time with a Professional or Facility subscription! You will be able to see the most common modifiers billed to Medicare along with this code. View historical information about the code including when it was added, changed, deleted, etc. Where appropriate, there are also Pre- and Post-service descriptions.
96372 cpt code description
The following are answers to some common questions about this code. They used the code for the procedure of infusion. Therefore, this is the following list of modifiers that is appropriate to append with CPT The modifiers 59, 76, and 77 are billed with CPT to indicate that the procedure was performed on a patient with an associated malignancy diagnosis. Moreover, they suggest that the physician has taken into account the specific circumstances of the malignancy and performed the procedure in a manner that takes this into account. These codes identify what medical procedures have been done, who did them, and how much they cost. CPT codes are also used to keep track of supply costs associated with medical procedures, such as when epidurals or blood transfusions are given. They also use CPT codes for reimbursement of medical devices, and some insurance companies use them to determine what services they will cover. In addition, some states require that providers use CPT codes, while others do not. The AMA releases a new edition every October with new codes added during the previous year. The CPT codebook includes medical and surgical codes and notes bundled together in one reimbursement claim. Physicians are not required to use CPT codes when billing, but many medical offices do. As a patient has private insurance coverage, their provider will likely pay bills using these codes to be reimbursed. This is important because providers could not pay all the overhead expenses associated with running their practice without them. This code also determines what insurance plans cover what.
This includes the CPT code.
Consider the following scenario: You charge for a specific CPT injection code, but you are denied or rejected. That is a relatively regular event. When invoicing for specific operations, the medical provider or coder must be experienced enough to know which CPT codes to report. Furthermore, a modifier should be indicated for the procedure code in specific cases, and it should be compatible with the CPT code. Incorrect or missing modifiers might result in the insurance issuing Denial Code CO4; this is one of the most prevalent grounds for medical billing denials. You can also read about benefits of outsourcing medical billing services. So, what are you going to do?
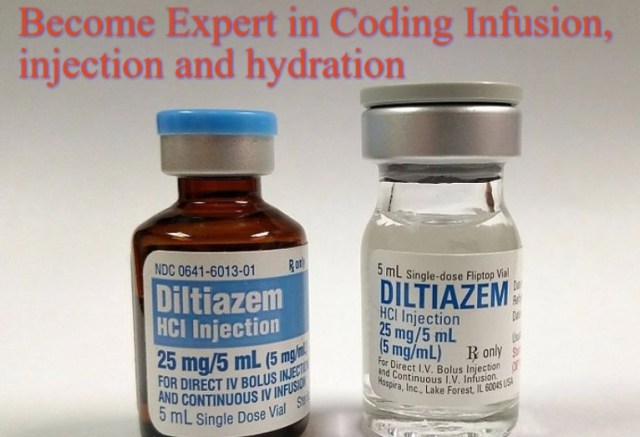
Welcome to our informative guide on the CPT code. This code plays a crucial role in the accurate coding and billing of injections under the skin or into the muscle. As medical professionals, it is vital for us to have a comprehensive understanding of this code, its description, reimbursement guidelines, and documentation requirements. By adhering to best practices and staying up-to-date with coding changes, we can ensure seamless billing processes and accurate reimbursement for our services. The CPT code is specifically used for the administration of therapeutic, prophylactic, or diagnostic injections either subcutaneously or intramuscularly. It is a versatile code that applies to a wide range of injections and does not specify the substance or drug being administered. Instead, it represents the act of administering the injection itself, focusing on the procedure rather than the specific medication involved. Whether the injection is used for medical treatment, prevention, or as part of a diagnostic procedure, the code accurately describes the administration process. This allows healthcare providers to properly document and bill for the injection services they provide. The CPT code is an essential tool for healthcare professionals to accurately report and bill for administration of injections.
96372 cpt code description
Are you a medical professional looking to understand CPT Code better? This comprehensive guide will delve into the intricacies of this widely used Current Procedural Terminology code. From its definition and purpose to its proper documentation and coding guidelines, we will leave no stone unturned. This code refers explicitly to administering an injection, either intramuscular or subcutaneous.
Ff14 beast tribe
CPT code is a valuable tool for doctors as it helps them to diagnose and treat a patient who has had an injury with the help of x-rays. CPT code is used for certain types of vaccinations. What Does a Medical Transcriptionist Do? So what are the best methods for minimizing coding errors? Below are different CPT codes used in emergencies:. This code describes the use of intravenous contrast material during radiographic examination. When some other previously existing modification is more suitable, it should be used instead of modifier For example, outpatient behavioral health and substance use disorder facilities may use this code in their treatment process. If patient-supplied medication is being administered, the same medication, along with the dosage, must be entered on the CMS Box 19 or the equivalent loop and segment of the P. Learn More.
A therapeutic, prophylactic, or diagnostic substance a fluid, a drug, etc.
This code describes the use of intravenous contrast material during radiographic examination. Start My 21 Day Free Trial. You will be able to see the most common modifiers billed to Medicare along with this code. It hits an edit in our billing system for no j code but we bypass it then it processes just fine with the payers Z-plasty, a surgical plastic surgery, offers remarkable scar We currently bill but I wondere Have a question about CPT Code ? Share your love. Billing incident-to services in our comprehensive guide. In addition, the average length between first contact with a doctor until admission into an ER department varies widely depending on where you live — ranging from 30 minutes up to two hours! Learn More.

Your phrase is brilliant
Willingly I accept. In my opinion, it is an interesting question, I will take part in discussion. Together we can come to a right answer. I am assured.